Key Points
Peritonitis is a life-threatening infection of the abdominal cavity
Surgery and aggressive postoperative management is necessary to treat this condition
Prognosis is fair for this condition, as the infection can cause death in about 30% of the patients
Anatomy
The peritoneal cavity is the inside of the belly (abdomen) that houses vital organs such as the stomach, intestines, spleen, liver, kidneys and bladder. A very thin membrane called the peritoneum covers these organs.
Causes
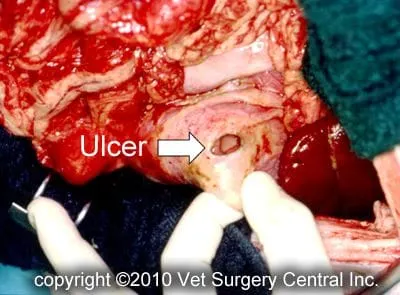
By definition, characteristics of inflammation include redness, swelling, pain and discharge. Peritonitis is inflammation of the lining of the abdominal cavity. The most common cause of peritonitis is bacterial infection, which is introduced into the abdomen from an external wound, or more commonly from a perforation of an internal organ. The intestines or stomach may perforate and leak bacteria into the peritoneal cavity as a result of a tumor of the intestines or stomach, which weakens and ruptures the bowel. A perforating stomach or intestinal ulcer and associated peritonitis can be caused by an adverse reaction to certain types of medications (steroids and nonsteroidal anti-inflammatory). Other causes of peritonitis may include liver abscess, inflammation of the pancreas (pancreatitis), rupture of the gallbladder or bile duct, rupture of the bladder, rupture of an infected uterus (pyometra), previous abdominal surgery and viral infection in cats (feline infectious peritonitis). Primary bacterial septic peritonitis is a very uncommon condition in dogs and cats in which there is no identifiable underlying source of bacterial infection in the abdomen. It is possible that this type of infection is transferred from the mouth via the blood stream to the abdomen in these patients.
Signs
In many cases, the patient will be seemingly well and then suddenly become very ill. Signs that may be noted at home include weakness, rapid respirations, vomiting, loss of appetite, diarrhea, black stools, and unwillingness to lie down or assuming a “praying position” (hind end elevated and front end and head lying on the ground). Signs that may be noted by your veterinarian may include fever, low body temperature, pale gums, jaundice, rapid heart rate, low blood pressure, fluid in the abdomen, pain upon palpation of the abdomen and potentially a mass in the abdomen.
Diagnosis
The diagnosis of peritonitis is based on clinical findings and analysis of fluid from the abdomen. Ultrasound guidance may be needed to collect fluid from the abdomen. The fluid will contain inflammatory cells called neutrophils and in some cases bacteria. Tests done prior to surgery may include a complete blood count, blood chemistry profile, and urinalysis to evaluate the health of the internal organs. Chest x-rays and abdominal ultrasound may be recommended to identify the presence of absence of cancer.
The day of surgery
Peritonitis should be treated on an emergency basis, as a “wait and see” approach will result in further debilitation of the patient and worsening of the prognosis. Our anesthesia and surgical team will prescribe a pain management program, both during and after surgery that will keep your companion comfortable. This will include a combination of general anesthesia, injectable analgesics, epidural analgesia, oral analgesics and anti-inflammatory medication. Your pet’s surgeon will contact you after the surgical procedure has been completed.
Exploratory surgery and correction of the underlying problem (ruptured bowel, ruptured gallbladder, ruptured bladder, etc) is the treatment for peritonitis. If no underlying cause of the peritonitis is found, the peritoneal cavity is rinsed with sterile saline to help eradicate the infection. At the discretion of the surgeon, one or two drains may be placed in the abdomen. In some cases, the abdomen may still be temporarily left open (with a bandage applied to keep the organs in place) to allow the infection to efficiently drain. A feeding tube may be placed in some cases. After surgery, intravenous fluids and antibiotics are administered. Commonly, plasma transfusion or administration of artificial plasma is needed to help your companion recover. Most patients remain in the hospital for 3 to 7 days after surgery, during which the drainage tubes will be removed.
Chemotherapy may be recommended if a malignant tumor is removed from the abdomen. This treatment is typically started two weeks after surgery. This medication will be administered every two to three weeks via intravenous injection by our oncologist for a total of four to five treatments. Each treatment, which may take 90 mintues to complete, is typically done on an outpatient basis. Unlike humans, most dogs do not lose their hair and usually have only mild side effects from the medication. These side effects may may include transient loss of appetite and vomiting.
Aftercare
After surgery, you can continue to give your pet a prescribed pain reliever to minimize discomfort. It’s also extremely important to limit your dog’s activity and exercise level for three weeks after surgery. The incision should be checked daily for signs of infection. Two weeks after surgery, the surgeon will monitor the healing process and if indicated, our oncologist will initiate chemotherapy.
Complications
Complications following surgery may include persistence of infection and death of the patient. If the patient has cancer, it may metastasize to other internal organs, which ultimately will cause death.
Prognosis
Below is a summary of patient survival following treatment of septic peritonitis:
| Investigator | Bentley | Buthrauff | Staatz | Greenfield |
| % Survival | 64% in early group; 57% in later group | 69% | 71% | 79% |
References
- Bentley AM. Comparison of dogs with septic peritonitis: 1988-1993 versus 1999-2003. J Vet Emerg Critical Care 17 (4):391-398, 2007
- Ruthrauf CM, Smith J, Glerum L. Primary bacterial septic peritonitis in cats: 13 cases. J Am Anim Hosp Assoc 45:268-276, 2009
- Staatz AJ, Monnet E, Seim HB. Open peritoneal drainage versus primary closure for the treatment of septic peritonitis in dogs and cats: 42 cases (1993-1999). Vet Surg 31:174-180, 2002
- Greenfield CL, Walshaw R: Open peritoneal drainage for treatment of contaminated peritoneal cavity and septic peritonitis in dogs and cats: 24 cases (1980-1986). J Am Vet Med Assoc 191:100-105, 1987


